Blog
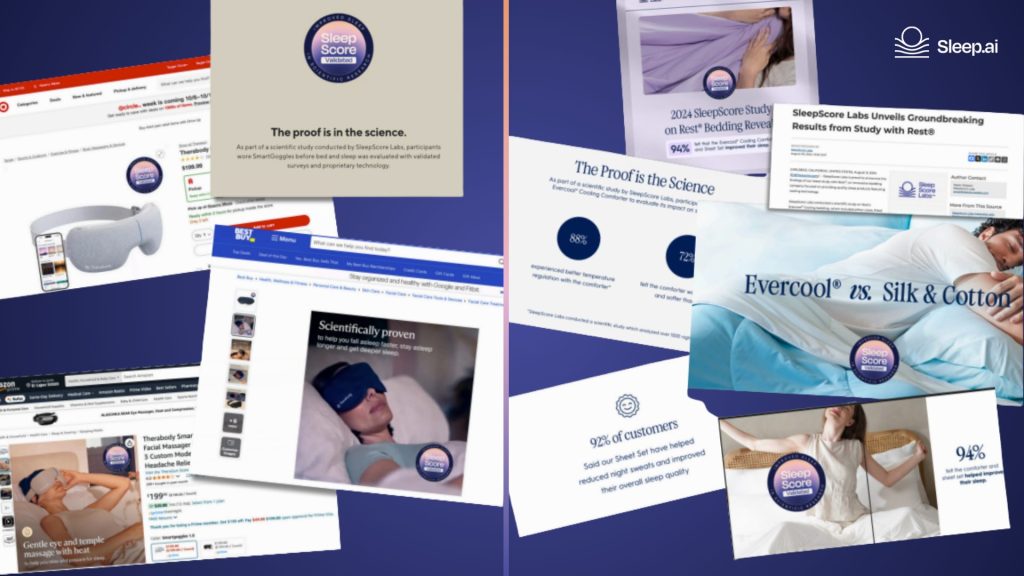
Validation Marketing: Why Your Study Should Be Your Strongest Sales Asset
When brands invest in scientific validation, they often focus on the study itself: the methodology, the metrics, the seal. But…
Introducing SleepScore
We deliver accurate data, actionable insights, personalized coaching and proven outcomes your customers need.
Sleep Insights
Last Published on 31st January 2022 by SleepScore Labs

As women approach their midlife stage, many experience problems getting high-quality sleep. This is attributed not only to menopause but also to perimenopause (transition to menopause) and postmenopause (after reaching menopause).
According to data from the National Health Survey Interview, 2015, women between ages 40 to 59 experience a wide range of sleep issues, including:
Similarly, data from the Study of Women’s Health Across the Nation (SWAN) shows that women are more likely to experience sleep disorders as they enter and during menopause, with the prevalence of sleep disorders being:
If you’re at the menopausal stage of your life and the idea of getting consistent healthy sleep seems like a long-lost dream, know that this is far from the truth! You can still maintain healthy sleep by incorporating certain habits and, in some cases, getting additional support from a healthcare provider, if necessary.
Menopause occurs when a woman’s ovaries no longer produce estrogen and progesterone, two main reproductive hormones in women. With these changes comes others—you may experience changes in your energy levels, mood, weight, sex drive, and sleep.
Most women experience menopause between ages 40 and 58, with the average age of onset being 51.
When it comes to changes in sleep, some of the contributing factors that may be at work include:
Vasomotor symptoms are more often referred to as hot flashes or flushes and are one of the most common symptoms women experience during menopause. Reports show that it happens to 75% to 85% of women during menopause. Vasomotor symptoms usually last for not more than 2 years after menopause, but some women may experience it for up to 10 years or more.
Hot flashes occur when a person experiences a sudden wave of heat, starting from the upper part of the body to the rest of the body, usually followed by sweating.
When hot flashes occur at night, they may disrupt sleep and cause multiple awakenings at night—impairing sleep continuity, one feature of healthy sleep. Hot flashes are also associated with the development of insomnia or may worsen insomnia symptoms in some cases.
The Journal, Sleep Medicine Clinics, describes insomnia as the “most severe clinical manifestation of recurrent and chronic perceived poor sleep,” and one out of four women report experiencing at least one symptom of insomnia.
Insomnia is a sleep disorder that occurs when a person regularly finds it hard to fall and stay asleep, even without any external disturbance.
Insomnia rate in women during menopause is 28–63%, according to different studies, with data showing that menopausal women frequently get less than 6 hours of sleep in 24 hours.
Insomnia, in the short term, may cause tiredness, restlessness, poor mood, irritability, low energy levels, slow response time, and in the long term, it is associated with chronic disorders such as obesity and heart disease.
Estrogen and progesterone levels begin to decline as a person enters menopause. And these drops have been linked with the likelihood of experiencing poor sleep.
An article published in the Journal of Menopausal Medicine explains the mechanisms that make estrogen and progesterone necessary for quality sleep:
Obstructive sleep apnea (OSA) is a common sleep-related breathing condition that occurs when the muscles in the airway drop intermittently during sleep, thereby inhibiting breathing.
Symptoms of OSA include excessive daytime sleepiness, fatigue, morning headache, loud snoring, irritability, and difficulty concentrating.
This disorder occurs in 17% and 34% of women and men in the US. However, studies suggest that obstructive sleep apnea is underdiagnosed in women.
Still, the prevalence of OSA in women increases as they enter menopause, with reports showing that it affects 47% to 67% of women during postmenopause. Weight gain and low estrogen and progesterone levels—occurring during menopause—may contribute to the development of this disorder.
Periodic limb movement disorder (PLMD) is a sleep disorder accompanied by repetitive and uncontrollable twitching and jerking of the legs during sleep and may impair sleep quality.
This disorder is common among women during menopause and may result from sleep apnea or anti-depressant medication use—also prevalent in women at menopause.
Restless leg syndrome is a sleep disorder characterized by an irresistible urge to move your legs during sleep.
This disorder occurs in 7 to 10 percent of people and happens more in women—especially those experiencing vasomotor symptoms—than men.
Women during menopause are at a higher risk of developing mood disorders such as anxiety and depression, and these disorders have been shown to affect sleep quality.
If your sleep quality has dwindled with the start of menopause, consider consulting with your doctor, who may best prescribe treatment appropriate for your case.
If you’re looking to improve your sleep health, here are some tips that may help: